Carter
A Whooping Cough Story
Carter’s story as told by his mother.
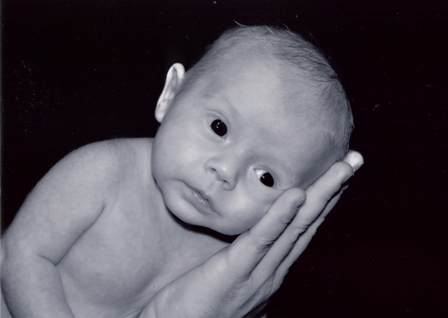
Landon Carter Dube was born December 8, 2009 at 5:08 P.M. by cesarean section. Our “Carterbug,” was three weeks early, weighed six pounds, six ounces and was 18.5 inches long. Carter was born breach. He had a head full of red hair; he was the spitting image of his daddy.
We spent Christmas and New Years as a brand new family of four.
We were careful who we left to hold Carter, where we took him because of the cold weather in South Carolina and the fear of the flu or swine flu.
Carter seemed healthy at his check-ups. At first, he was a little slow at gaining weight but quickly caught up, becoming a little chunky monkey. On January 15, he went in for his six-week check-up (although he was only five weeks and three days old). Our doctor was excited Carter had gained a little over a pound.
We had some concerns that Carter had been spitting up a little and seemed to be cranky at night. The doctor suggested switching his formula and monitoring his crying in case it was colic.
The first few days, Carter didn’t seem to spit up or cry throughout the weekend, so we assumed he was feeling better.
On Monday, Carter began to spit up again, only this time it seemed to occur a little more frequently. We weren’t alarmed because his pediatrician had said we could expect a little spitting up from changing his formula. Monday proceeded smoothly and Carter slept through the night.
On Tuesday, January 19, Carter was not himself; he was cranky and wasn’t satisfied unless we held him.
We tried a couple of methods to help calm him down that had worked in the past, but nothing seemed to help. When I took his temperature, I noticed he was running a low grade fever of 100.1, so we took him back to the pediatrician. Daryl (my husband) and I were joking about how overprotective we were acting and how it was probably just a little cold.
We saw a nurse practitioner that day; she was immediately concerned with Carter’s breathing rate and thought he may be a little dehydrated. The next thing I knew, we were in an ambulance, heading to Levine’s Children’s Hospital in Charlotte, North Carolina.
We were admitted to the eighth floor, the Progressive Care Unit, for observation. Doctors came in and asked a lot of questions over and over again. Everyone had to wear a mask and a gown because they were unsure as to what was wrong with Carter. The doctors threw around diagnoses such as RSV, pneumonia, an upper respiratory infection or pertussis (whooping cough). The whole family had allergy issues and mild colds, but we were all being treated for them; I had even been on antibiotics for seven days.
Over the next two days, Carter had to be put on nasal oxygen, was taken for chest x-rays and had his nose and lungs suctioned; they even beat his back to loosen up his lungs. Nothing worked and Carter began to act aggravated. They placed an IV in his arm (covering the finger he sucked on) to supplement his lack of milk intake.
Thursday, January 21 was a better day.
Carter ate well all through the night and the doctor decided if his progress continued, we could go home as early as Saturday morning.
On Friday, however, Carter started coughing again, lost his breath and turned blue. I totally panicked; if my husband would not have been there, I don’t know what would have happened. I just froze in my steps.
On Saturday, Carter was sent to the sixth floor, the Pediatric Intensive Care Unit, for better care and observation.
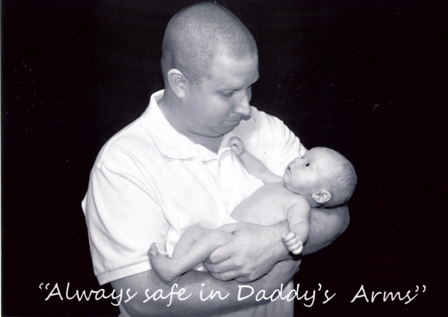
It was wonderful for Carter to have his own nurse who made him her priority. I was even able to cuddle with him and tell him about all of the things we were going to do once we got home. Daryl and I would take shifts staying up with Carter; we never wanted him to be alone and not see one of us there with him.
By early Sunday morning, the decision was made to put Carter on a respiratory machine.
He had become fussy and inconsolable, which caused him to struggle even more when he breathed. We didn’t know it at the time, but that was the last time we saw our Carterbug awake.
The next few days were like a roller coaster.
Later on Sunday, he was put on an Oscillator because he wasn’t strong enough to handle the respiratory machine. By Monday, January 25, we became hopeful that Carter’s condition had improved. We had family came visit and talk to Carter as though he was awake. We wanted Carter to stay aware of what was going on around him.
On Tuesday, Carter started going downhill.
Doctors were confused as to why Carter’s heart rate was extremely high and his blood pressure so low. By this time, Carter was the talk of the floor. We had three Pediatric Intensive Care Specialists, an Infectious Disease doctor, a Hemoglobin/Cancer doctor and enough residences and interns to fill a football field.
Around noon on Tuesday, the doctors discussed the idea of putting Carter on an ECMO (heart and lung bypass machine), as a last resort. We were told that if it was decided to put Carter on the ECMO machine, there would be a 60-40 chance that he would leave the hospital with us.
We discussed our options with the doctor and made arrangements for Zach to come and see Carter before the procedure was done. Zach, being only 10, handled the news very well and acted like such a trooper through it all. Carter went into surgery later that evening while we sat around with our wonderful family and friends and waited. It took about three hours for the procedure to be complete, but we were told Carter came through it ok.
I was not prepared for what I saw when I walked back to his room.
My sweet baby boy had huge tubes in the sides of his neck while blood pumped in and out of them. The ECMO machine itself required two people to run it at all times. Now Carter had four people in his room at all times, including two full-time nurses and two ECMO technicians.
Carter started to swell and wasn’t putting out enough urine for the fluid he was taking in. The doctors told us it was related to the stress on his body for being so sick. Now we had to worry about kidney failure and other issues related to the swelling.
Carter held his own on Wednesday, January 27 with no sudden changes to his condition.
It was the first day we relaxed a little and talked about a long term plan. They didn’t sugar coat it, we were still looking at a month or more in the hospital before we could take him home. When we went to bed Wednesday night, it was the first time I didn’t feel like I was carrying the weight of the world on my shoulders.
That feeling lasted about seven hours when we got a call from one of the specialists around. Carter had a rough night and they had to give him fluid boluses to keep his pressure up. The doctor explained that there were four more medicines they had available that could help Carter. After that, the rest was up to him. They started him on two of the medicines and we waited to see what would happen.
It was hard to stand back and look at my sweet baby boy swollen to nearly twice his original size. They had him under a heat lamp and two huge medicine trees held all of the medicines that were working to keep him alive. It is difficult to forget the machine that was also monitoring his heart and blood pressure which was constantly chiming, alarming us that something wasn’t right.
It was like a bad dream where we just couldn’t wake up.
We had asked the doctors to always be honest and to let us know when it got to the point that they were doing things to Carter and not for him.
We called our family in and asked them to come meet us at the hospital. Around 2:00 P.M., the third medicine was administered to Carter, but he seemed barely able to hold on.
At 3:00 P.M. on January 28, the doctor informed us about the last medicine they had available.
This medicine wasn’t used very often and was a last ditch effort, but if it worked, Carter could stay on it to get him over this hump. By this time, they are treating him for everything: whooping cough, fungal infections, pneumonia, anything they could think of.
We talked to our family about the medicine and decided to give it to Carter. It was like signing our lives away because the doctors had told us the medicine would tint his blood and skin blue. We signed many papers in preparation for the expected side effects.
The medicine was administered around 3:30 P.M.
After about 30 minutes, we didn’t see a great change, but the doctor wanted to give him more time. We waited a little longer, until our doctor approached us and said that it was now in Carter’s hands.
Daryl and I began to let our family go back to say their goodbyes to Carter. It was the longest walk to take over and over again with our family, as their hearts broke along with ours.
At this point, Carter’s condition had gotten worse.
His IV in his foot was blown and they were not getting a good reading of his blood pressure. His kidneys had completely stopped working and his body was too fragile to handle dialysis.
We asked our preacher to pray with us and Carter for God to hold him close and not let him be afraid. I talked to Carter and told him how much we loved him and how excited we were when we found out we were pregnant with him. There was so much we wanted him to see and so many people that hadn’t had a chance to meet yet.
I held his hand, the only thing I could touch that wasn’t wired to a machine, and told him that I loved him very much.
I told him how brave he was and how he had fought a great fight, but if he was tired and wanted to go to heaven, he should go. I told him that momma and daddy would miss him, but we would see him again one day. Carter showed us that he was ready to go to heaven and not hurt anymore.
At 5:06 P.M. on Thursday January 28, Carter received his angel wings. He went peacefully on his own terms to the arms of Jesus. I truly believe that we will see him one day and that his spirit carries with us every day.
BECOME A VACCINE ADVOCATE
There are lots of ways you can make a difference in your community.

